Directed evolution of multiple genomic loci allows the prediction of antibiotic resistance
Given the ever-increasing threat of antibiotic resistance, researchers of the Biological Research Centre of the Hungarian Academy of Sciences have developed a method to rapidly test new antibiotic candidates for their potential to be hit by emerging resistance. The high-throughput mutagenesis method, dubbed DIvERGE, reveals probable resistance within days, making it a fast and cost-effective tool to guide antibiotic development. Moreover, DIvERGE has widespread biotechnological applications including the directed evolution of enzymes and biosynthetic pathways.
The research, published in the June issue of the Proceedings of the National Academy of Sciences of the United States of America, builds on targeted modifications of bacterial DNA. It rapidly screens the evolutionary changes of the microbial genetic material and identifies those that can lead to resistance against antibiotic treatments. The method, called ‘directed evolution with random genomic mutations’ (DIvERGE), allows up to a million-fold increase in mutation rate along the full length of multiple pre-defined loci in numerous bacterial species. Thus, it requires only one day to generate billions of mutation combinations which can result in resistance to an antibiotic-of-interest. Although the exact probability and the time-frame of resistance emergence require further analyses and should consider other factors as well, this ability to rapidly analyze potential antimicrobial resistance (AMR) processes could be a powerful strategy to guide drug development.Please click here to read the full article.
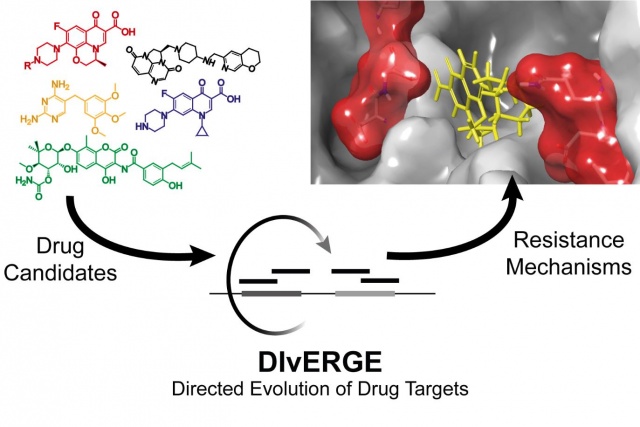 Directed evolution of antibiotic targets enable rapid identification of resistance mechanisms. Image from Akos Nyerges (http://group.szbk.u-szeged.hu/sysbiol/pal-csaba-lab-member.html#akos-nyerges)
Directed evolution of antibiotic targets enable rapid identification of resistance mechanisms. Image from Akos Nyerges (http://group.szbk.u-szeged.hu/sysbiol/pal-csaba-lab-member.html#akos-nyerges)Wide range of potential applications
Moreover, DIvERGE addresses several unmet needs in basic and applied research. First, it promotes the directed evolution of multiple genes in their native genomic context. Directed enzyme evolution resulting in improved protein characteristics (such as higher enzyme productivity or improved thermostability) has special importance in synthetic biology and biotechnological applications. Also, the researchers predict that DIvERGE will be applicable to optimize metabolic pathways and synthetic DNA segments. Finally, DIvERGE could also be applicable to investigate key issues in evolutionary biology.
Proof-of-concept tests regarding antibiotic resistance
As a proof of their concept, the research group from the Biological Research Centre of the Hungarian Academy of Sciences tested the assay in several bacterial species and against various antibiotics, including two widely used drugs, trimethoprim and ciprofloxacin, and a drug candidate that is under clinical development. Their results confirmed that DIvERGE can detect resistance processes that had been previously described in clinical isolates. Within a single screen, DIvERGE precisely detected the known ciprofloxacin resistance hot-spots, and even revealed some other resistance-conferring mutations at novel sites in E. coli. Interestingly, the assay also revealed major differences in the effects of resistance mutations between pathogenic and non-pathogenic strains. This observation underlines the importance of directly studying the resistance profiles of relevant pathogens and can pave the way towards pathogen-specific therapies.
Also, the research team predicted the probable emergence of a high level of resistance to gepotidacin (GSK2140944). Gepotidacin is a novel antibiotic with a novel mode of action compared to existing antibiotics and is currently in phase II clinical trials. Within days, DIvERGE revealed that a combination of two specific mutations is sufficient to produce dramatically high resistance to this novel drug in pathogenic bacteria.
Extremely fast and cost-effective guide to drug-optimization
“Importantly, our goal is not to lose a drug candidate, but rather to draw attention to the risk of AMR and offer information to mitigate resistance development after a drug reaches the market. By revealing possible routes to resistance development, our aim is to give a chance to find better therapeutic solutions that can slow the loss of effectiveness for these valuable, new antibiotics”, explains Akos Nyerges, the first author of the paper and the developer of DIvERGE. “Compared to other available methods, DIvERGE is extremely fast, highly cost-effective, and can be readily applied in numerous bacteria with medical and industrial relevance. The assay enables preliminary resistance testing of lead molecules within days, at a cost of about 50 to 100 USD”, he adds. “Thus, it is a potential tool to reinvigorate drug development, eliminating many dead-end attempts and saving millions of dollars.”
Promoting antibiotic development
Regarding the potential applications of DIvERGE, Csaba Pal, Ph.D, leader of the research group, highlights another important consideration. “The possibility to screen the resistance profiles of antibiotic compounds in a cost-effective and high-throughput manner is a significant incentive in the research for novel antibiotics. The fear from the rapid emergence of resistance is a large obstacle to new antibiotic development as no one can predict the time-frame until a newly approved antimicrobial drug would become ineffective. Once it happens, the chance for the drug to make profit disappears, and no pharmaceutical company is willing to invest in a loss-making product. However, by revealing potential resistance-mechanisms, DIvERGE could guide computer-aided drug design to help avoid these resistance-promoting features. Therefore, DIvERGE could allow pharmaceutical companies to expand the time-frame until potential loss of effectiveness and make antibiotic development more profitable.”
As part of global antibiotic awareness, a September 2017 report of WHO (“Antibacterial agents in clinical development – an analysis of the antibacterial clinical development pipeline, including Mycobacterium tuberculosis”) highlights a serious lack of new antibiotics under development to combat the growing threat of antimicrobial resistance. The new test method of the Hungarian research group might be a breakthrough advancement in terms of promoting and directing antimicrobial research.
